Enabling effective patient discharge from hospital to community health services
The discharge process involves transferring a hospital inpatient to care in their home, supported by community nursing and care staff. In a recent project between Livework and the Sussex Community NHS Foundation Trust, we explored how aligning real-time electronic data flows and processes for medically ready to discharge patients could help redesign the discharge process.
We focused on three key factors:
-
Redesigning data flows and processes for medically ready to discharge patients from hospital to community providers.
-
Understanding the staff and patient experiences of the discharge process – identifying what worked well, the pain points, needs, and opportunities that would have the greatest impact on care.
-
Documenting the data collected in the discharge process, enabled the digital team to design the data architecture to support a more effective handover of patients from hospital to home.
The patient view: challenges during discharge from hospital
Some patients awaiting discharge from hospital to home were unsure about the care they would receive post-discharge. There were delays in the data shared during the handover between hospital and community staff. This meant that when patients moved back to their homes, they were not clear about the care management plan or who would be caring for them.
Services were not tailored to meet patients’ specific needs – e.g., transport requirements or preferred forms of communication (verbal, digital, or paper). Staff need to access data to inform how and when to deliver services, as well as communicate care management plans.
More detailed and timely information about patients’ needs and preferences could reduce waste of resources, and support safe and efficient transfer of care.
Five things we learned: the staff view
We conducted in-depth qualitative interviews with staff to obtain a deep understanding of the discharge process and their experience. Our recommendations include:
- Retain the Discharge Hub: Staff recognised that the existing Discharge Hub improved communication and streamlined processes. We were careful to build from this perceived success.
- Reduce data duplication: The same data were collected in multiple ways, in both the hospital and community & could be rationalised so that data were only entered once.
- Provide timely information to plan and predict flow: Community staff did not have access to information about patients who would need their services after discharge from their hospital stay. It was difficult for them to understand the numbers of patients planned to leave hospital & their needs to manage their future workload and allocate staff with the right skills to meet demand.
- Use predictive algorithms: Enable community staff to analyse demand to enable staff to plan for community resources accordingly.
- Adopt digital innovations: Develop and execute a suite of small scale digital innovations to test assumptions about how discharge to patients’ homes can be achieved more efficiently.
Service design as connective tissue of digital delivery
Service design enabled a collaborative environment which brought staff and patients’ perspectives together.
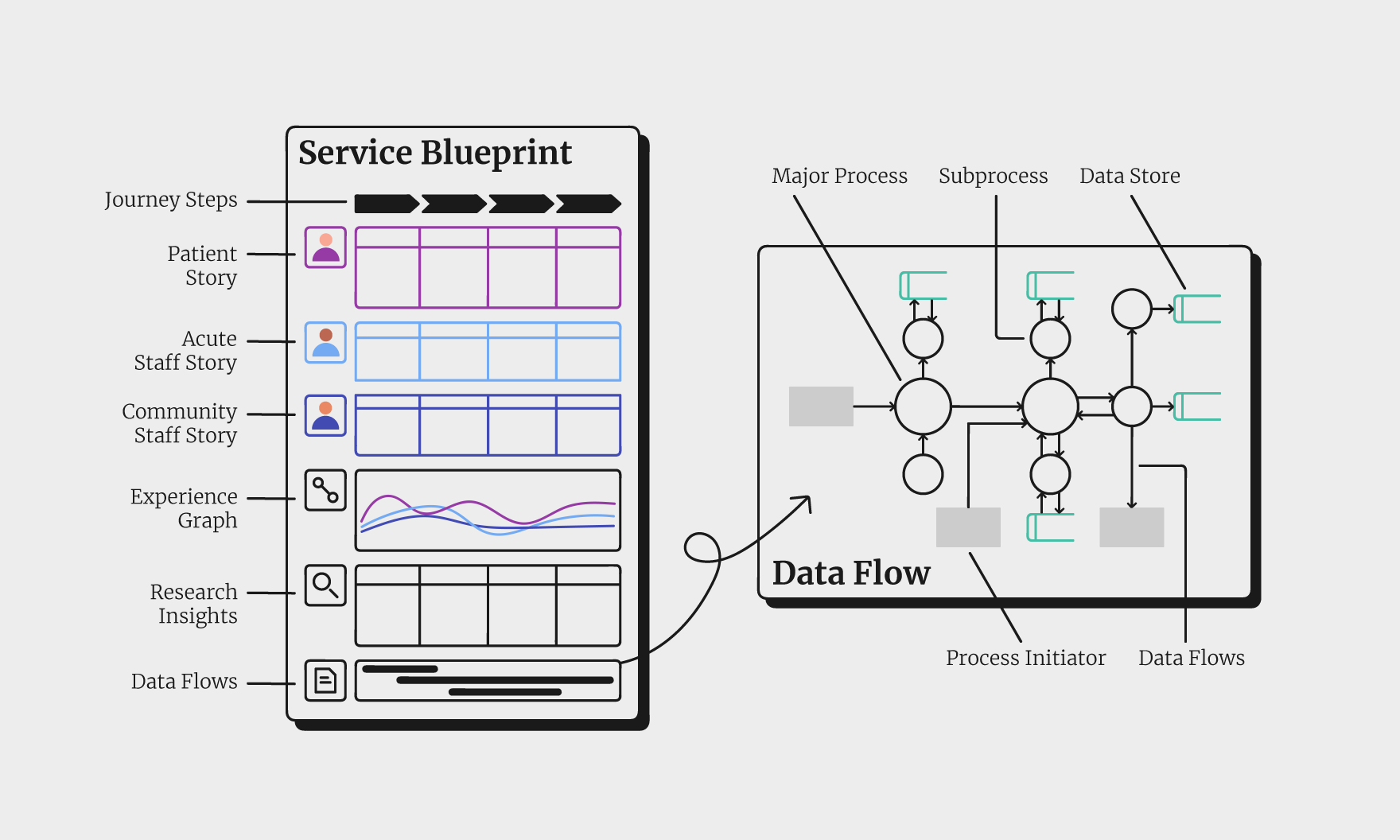
We visualised opportunities in the service blueprint & future data flow scenarios between the two Trusts. Rather than implementing a ‘big bang’ approach, small scale digital innovations could be tried, which helped to manage risk.
Grounding the research in patient and staff experiences brought a human perspective to the solutions, capturing their expectations and ideas for change.
Working from the visual representations of the blueprint and data flows, we were able to inform the future data architecture and the opportunities for redesign of the discharge process.
Recommendations covered strategic and operational areas beyond digital solutions, including other service areas which would benefit from this approach, for example Hospital at Home or Virtual Wards.