Healthcare staff are frustrated with current EPR systems across many different digital platforms
The COVID-19 crisis accelerated the need to interact with patients through digital channels. Clinical and administrative healthcare staff quickly adapted to working remotely [3]. They used the existing EPR systems to access patient information and plan their care. However, this highlighted the frustrations that staff felt as it took time to navigate the EPR systems, find the right information, and then check if it was accurate. This also highlighted the need for a modern EPR system that would allow staff to communicate with their patients, while integrating with apps to enable patients to monitor and manage their own care.
To address the need to modernise EPR systems, NHSX released the Digital Aspirant Plus Programme. Its goal was to provide additional funding to support NHS Trusts to accelerate their digital transformation journey [4]. This was the focus of Livework’s project with the Sussex Community NHS Foundation Trust (SCFT), the first NHS Community Trust to receive funding to participate in the EPR Innovator Project for Mental Health and Community Trusts.
SCFT recognised that, in order to improve the use of an EPR solution in community health services and Intermediate Care Units (ICU), there was an opportunity to conduct user research to understand the needs of their staff. The research identified their pain points and frustrations with the current system. It showed opportunities for development to support healthcare staff to improve how they worked as a multi-disciplinary team (MDT). SCFT used the research to write a business case and a specification of requirements to set in motion improvements to SystmOne.
Five things we learned from healthcare staff
-
Improve usability: Several staff members noted that they would like SystmOne to be easier to use and navigate. Issues included being too click-heavy, not visually appealing, or intuitive — in that there were different ways to do the same thing. There were also multiple places to input information and if you did not know where the information was stored, it would be difficult to find. The mobile app version of SystmOne did not have the same functionality, therefore staff were less likely to use it.
-
Integrate data, in real-time, from systems outside of SystmOne: Healthcare staff noted that the GP system had Read codes. The version of SystmOne in the Intermediate Care Unit (ICU) did not, which made it difficult to search for a diagnosis. It was noted that it would be sensible to have these same Read codes in the (ICU) version of SystmOne. The acute (hospital) systems were also not integrated into SystmOne. Having the ability to view patient data across GP practices, community teams, and the acute (hospital) systems would save time. The workaround for this involved making phone calls to multiple staff teams. SCFT is currently developing a shared care record (Plexus) that could grant everyone within a locality access to the same information – with patient consent.
-
Reduce duplication: Staff members reported that they were repeatedly entering the same data, being unable to dip in and out of assessments. If they left a page, they could not go back in and a new document would be created. This resulted in a duplication across several assessments. For example: There is a physiotherapy assessment and a doctor’s assessment, with similar data on each not being pulled through from one template to the other. In many cases, this data could be combined.
-
Create auto-population functionality: There are a series of customised templates that have been created within SystmOne for different healthcare practitioners. Initially, the templates led to improved ways of working, saving time in the process. However, healthcare staff have since recognised that there is an opportunity to auto-populate information across internal teams using SystmOne. At the referral stage, this would enable clinical and administrative staff to confirm that the information is correct, as opposed to going through a lengthy registration process with the patients.
-
Reduce excessive pop-ups: While using the system, staff experience a constant barrage of pop-ups — asking ‘yes’ or ‘no’, or ‘save’ — which is not needed in a busy environment.
Five things we learned about patients’ use of apps
-
Apps were not suitable for some patients: Especially those who were frail or had a condition that precluded them from using an app.
-
Some patients want to use apps to control and manage their health, or the health of a family member: They want a timely and responsive service that helps them manage their own care at home
[5]. For some patients, this meant that they did not need to go in for an appointment if they could monitor and record their condition at home. They could then have a video conference with a healthcare professional, taking away the need to travel. A patient noted that if the app was working perfectly, it would be ideal to have the data sent to the healthcare team and be reviewed remotely, rather than setting up an in-person appointment at a later date.
-
Apps were viewed by patients as a useful tool for rehabilitation at home: Patients gave examples of using apps to follow exercises at home to improve their condition, noting how easy it was to follow someone showing them what to do. Patients also stated that they preferred to be at home. However, there were frustrations when inputting data into an app. For example: A patient noted that it would be easier to input numbers as digits, rather than using the current method of a slider. In addition to this, the instructions to use apps needed to be clearer.
-
Patient notes need to be transferred automatically across localities: There is an expectation from patients that when they move areas or services (i.e., from children to adult services), that their notes are transferred automatically and that whichever health professional is caring for them can see these. Patients told us about instances when their notes could not be carried across and felt this created an obstacle that did not need to be there.
-
An interactive EPR system could improve patient engagement: Both staff and patients spoke about how an EPR could offer a more interactive platform for patients to engage with clinicians. Especially if it was integrated with apps and other media (e.g., videos). An EPR could support patients to monitor their condition and motivate them to undertake health management actions identified in their care plan (e.g., following physiotherapy programmes or speech therapy exercises).
Service design as the connective tissue between User Centred Design and EPR adoption
Service design is the connective tissue. It is not only a methodology, but provides tools and values to help people challenge their thinking.
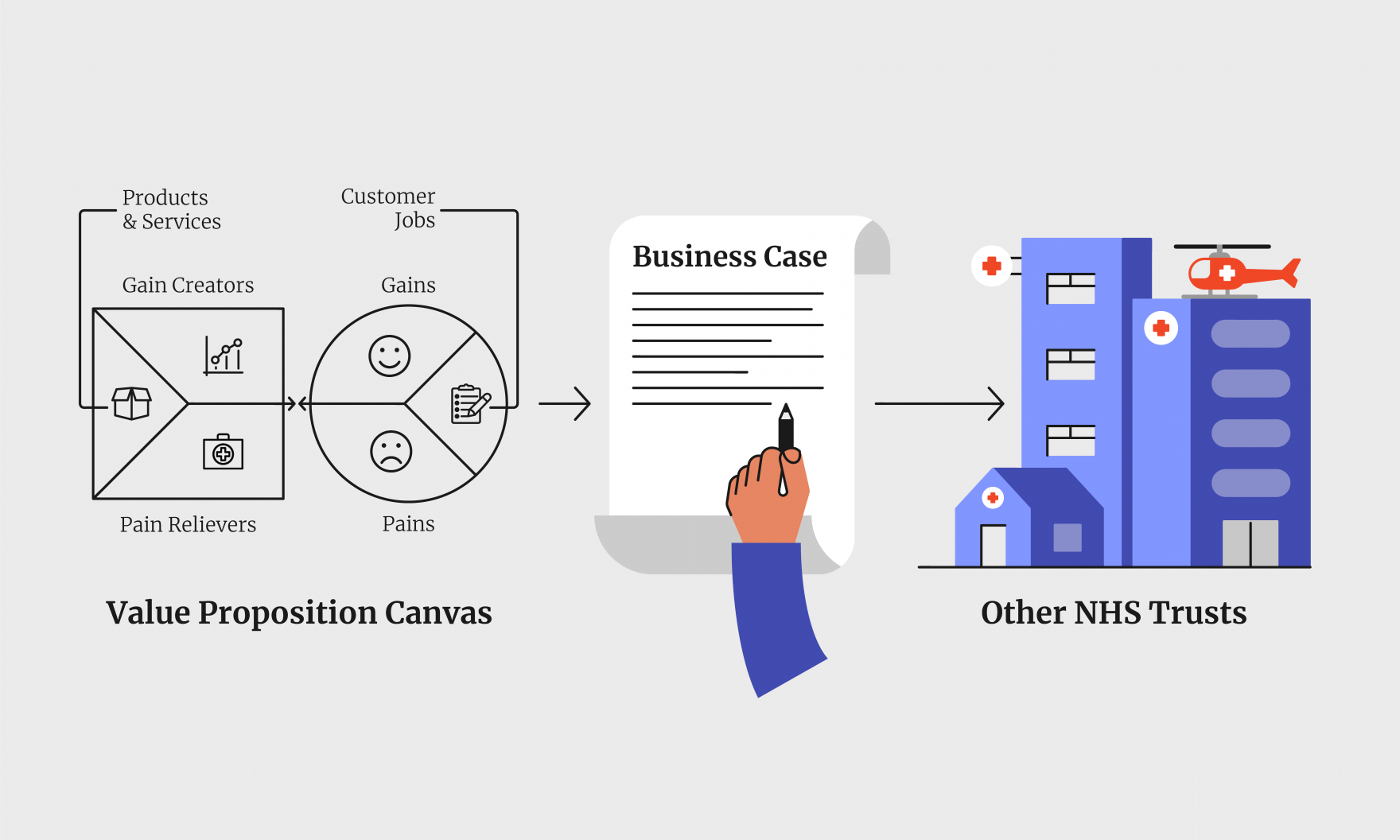
A key tool that we used as part of our research was the Value Proposition Canvas. This framework describes the features we are designing to address, the staff jobs to be done, the user gains (benefits), and any pain points. Also included is a description of the products and services that are currently in place, as well as future opportunities to improve these. The Value Proposition Canvas enabled us to understand and capture this in relation to using an EPR system. It showed the fit between what staff and patients needed, and what a modern EPR could actually offer.
Through in-depth qualitative interviews, we obtained an understanding of what healthcare staff and patients were looking for in an EPR. We designed a service blueprint to map the clinical journey and the potential opportunities for improvement. We also created logical data flow diagrams to show how data is used and stored. This highlighted the need for sharing data across healthcare teams, to ensure that patients received the right care at the right time. We then validated our insights with a staff survey across Community and ICU teams, receiving over 100 responses.
We identified that the needs of staff centred around the access to data and its integration — both within and across organisations, data systems and apps. For example, one community staff member stated the following: “It would be good to have Discharge Planning notes and see the acute (hospital) data, to be able to plan the caseload. It would be a big help, but hard to achieve. Perhaps the Discharge Team connected to our team could have access to it.”